Neuronoff, Inc., a pioneer in minimally invasive neuromodulation solutions, announced two major funding milestones totaling $5 million to advance its innovative Injectrode® technology. The Department of Defense (DOD) has recommended $1.73 million to fund a clinical randomized controlled trial (RCT) for the treatment of neurogenic bladder following spinal cord injury, while the National Institutes of Health (NIH) has awarded $3.2 million to support preclinical research in overactive bladder treatment.
The DOD funding will support a clinical randomized controlled trial in collaboration with the University of Texas Health Science Center in Houston, TX. This three-year clinical evaluation, titled “Home Neuromodulation for Neurogenic Bladder Management in Spinal Cord Injury: A Hybrid Implementation-Effectiveness Trial,” will assess the Injectrode’s safety and efficacy when implanted along the tibial nerve in individuals with Spinal Cord Injury (SCI).
Related: AVS secures $36m to support US launch of Pulse IVL device
The study introduces Injectrode Tibial Nerve Stimulation (iTNS), evaluating its implantation process, measuring treatment effects through an 8-week self-administered protocol versus sham treatment, and investigating its mechanisms of action. Using the Injectrode as the active intervention, the study will measure both the complete elimination of overactive bladder (OAB) medication and the percentage reduction in OAB medications from baseline to study completion. As the first-in-SCI human clinical trial, this phase 1/2 study will provide crucial data for FDA presubmission engagements and inform the design of subsequent pivotal trials.
“Neurogenic bladder is a major complication in spinal cord injury. Current therapeutic approaches lack long-term reliability and suffer from drug-based side effects,” said Dr. Argy Stampas, MD, lead PI for the clinical RCT study. “To achieve stable tibial nerve engagement for years to come, traditional neuromodulation solutions require some level of open cut-down to the nerve, a step that should be avoided to ease and broaden the therapy access for patients. The Injectrode’s needle-based delivery and simple removal pathway is expected to lower the risk for patients and has the potential to provide a more cost-efficient path, enabling wider clinical adoption of the future therapy.”
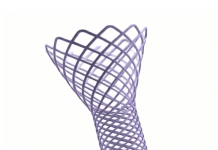
In parallel, a preclinical R01 proposal titled “An Injectable Electrode to Better Isolate the Posterior Tibial Nerve to Treat OAB” received a five-year, $3.2m grant from the National Institutes of Health. This collaborative work between the University of Wisconsin (UW), Case Western Reserve University (CWRU), and Massachusetts General Hospital aims to improve treatment for people suffering from Overactive Bladder (OAB) using the Injectrode’s innovative two-component, passive injectable electrode system for direct nerve interfacing and improved target engagement. The study teams anticipate that this method will dramatically improve the reliability of the nerve interface resulting in better long-term stability while reducing complications.
Dr. Kip Ludwig, lead PI on the preclinical OAB grant, stated, “I’m excited at this opportunity to validate and optimize an innovative injection tool with embedded fiber optic for visualization, to optimize minimally invasive electrode placement for stimulation of the posterior tibial nerve to treat overactive bladder. This paradigm has the potential to revolutionize how neuromodulation procedures are performed.”
These new grants bring Neuronoff’s total secured funding to $9.1 million, demonstrating strong federal and state support for advancing elegant, micro-invasive neuromodulation therapies. Previous funding includes grants from NIH HEAL, DARPA, Ohio Third Frontier Research, and the IQT In-Q-Tel EEI program to commercialize technologies.
Neuronoff’s CEO, Dr. Manfred Franke, stated in response to the latest news “We appreciate the continued state and federal investment in developing micro-invasive neuromodulation therapies for chronic conditions. Currently, neurostimulation is primarily a ‘therapy of last resort’ due to invasive surgical requirements and associated costs. Our elegant, needle-based approach to inject a self-anchoring lead enables chronic therapy options ranging from pain to autonomic, bladder and cardiac uses. By allowing patients to try neuromodulation as easily as a drug injection, while reducing healthcare system costs by a factor of 3 to 5, we aim to broaden patient access through a solution that benefits patients, physicians, providers, and payers alike.”