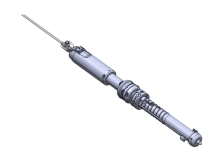
STIMIT AG is enrolling patients in a U.S. Food and Drug Administration Investigational Device Exemption (IDE) clinical trial designed to evaluate its noninvasive diaphragm neurostimulation technology.
STIMIT’s therapy aims to preserve diaphragm thickness in patients using invasive mechanical ventilation (MV) and are at risk of diaphragmatic dysfunction/atrophy. “STIMIT ACTIVATOR 1 PIVOTAL STUDY” will evaluate the safety and effectiveness of the technology for this indication.
Related: Mainstay Medical study demonstrates benefit of neurostimulation for back pain
The diaphragm is the body’s core breathing muscle and its fibers are lost by 50% in three days when patients on mechanical ventilators do not breathe on their own (Levine et al. 2008). Maintaining diaphragm activity is critically important to rapidly wean patients from mechanical ventilation (Morsy et al. 2015; Goligher et al. 2019), as patients on prolonged mechanical ventilation cost the U.S. healthcare system more than $16 billion (Zilberberg et al. 2012).
“STIMIT Activator represents the world’s only early-intervention, completely noninvasive therapy undergoing an IDE study designed specifically for diaphragm stimulation which is intended to induce inspiratory efforts in critically ill patients,” said Dr. Laurent J. Brochard, M.D., principal study investigator and head of the Interdepartmental Division of Critical Care, University of Toronto. “Diaphragm activity and the physiological approach to breathing is of utmost importance for any ICU patient and for hospitals aiming to liberate their patients earlier in a better state.”
In a broader picture, diaphragm stimulation may have potential benefits at the interface to the lung (physiological pressure distribution), as well as the brain (activate and preserve cells in brain areas responsible for breathing), and the heart (venous backflow) (Morris et al. 2022), requiring further research.
“Our vision for STIMIT goes far beyond this initial therapeutic application under investigation,” STIMIT CEO Ronja Müller-Bruhn stated. “Our earlier feasibility trials with anesthetized, healthy, and critically ill patients showed promising data that the STIMIT technology could ventilate patients in the future…that is, to noninvasively support moving air in and out of the lungs using physiological diaphragm breathing of a patient. This, of course, has enormous potential for ventilation and critical care.”
Patients are being enrolled at Beth Israel Deaconess Medical Center (BIDMC), a teaching hospital of Harvard Medical School; Yale New Haven Hospital (YNHH), the primary teaching hospital for Yale School of Medicine; UVA Health University Medical Center, a teaching hospital of University of Virginia School of Medicine; and, St. Michael’s Hospital, a Canadian teaching and research hospital of Unity Health Toronto.
The STIMIT Activator 1 is limited by U.S. law to investigational use.
Headquartered in Biel, Switzerland, and operating another site in Zurich, STIMIT was founded by Müller-Bruhn and Oliver Müller in 2018. The company develops non-invasive technology designed to activate and preserve diaphragmatic “breathing” muscles of ventilated patients who do not breathe on their own. Initial clinical data has already been collected in collaboration with clinics in Switzerland, and Germany, and additional data will be forthcoming from the U.S. randomised controlled multi-center trial.