What was once a taboo topic, male infertility is becoming more openly discussed between couples planning a family and with this a string of emerging technologies are in development to diagnose male infertility.
Starting a family is the decision of both prospective parents but infertility, a disease of the reproductive system, impacts the lives of millions of couples trying to conceive.
According to the World Health Organization (WHO), one in every six people worldwide will experience infertility in their lifetime. Historically there has been a stigma attached to infertility, but as more medical solutions appear on the market, the taboo is being slowly wiped away.
There is an increasing number of solutions to diagnose male infertility. One device from a Lithuanian company Caerus Biotech, a subsidiary of GryNumber Health Group, provides a sperm diagnostic testing solution designed to assess oxidative stress levels by clinicians.
The company sells around 50,000 tests a year at €100 ($105) to €150 ($158) per test and can prevent the need for in vitro fertilization (IVF) – one the most common types of assisted reproductive technology (ART) – in the future which can range between £5000 ($6085) and £6000 ($7302).
According to GlobalData’s market model, the consumable assisted reproductive technology (ART) devices market is forecast to grow at a compound annual growth rate (CAGR) of 6%, with the global market value surpassing $440 million by 2030. These results are driven by the age of conception, devices on the market and emerging technologies.
Martynas Linkevičius Chief Commercial Officer at Caerus said: “What was considered good sperm 20 years ago, does not meet today’s standards. These thresholds have drastically fallen with each edition of the WHO guidelines. There was a study here in the Baltics, on young military men. It showed the sperm concentration motility has been decreasing drastically. This is also experienced globally so male fertility is becoming a big issue.”
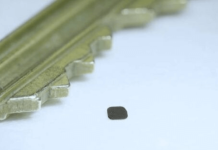
The sperm diagnostic device, MiOXSYS (Male Infertility Sperm Oxidative System) takes less than five minutes and requires minimal training. It measures oxidation reduction potential (ORP) and uses that data to help diagnose infertility.
The stigma
The stigma of male infertility casts a dark shadow over many. Society has ingrained the belief that a man’s virility was the measure of his worth, making it incredibly difficult for men to admit their struggles with infertility.
As more males share their experiences and struggles, the stigma surrounding male infertility is dissolving. Society is realising that infertility is not a reflection of a man’s masculinity, but a medical condition like any other. The cultural background of an individual also adds to this stigma but it’s shifting.
According to Caerus, there is a lot of interest in the diagnostic device from the Middle East, a traditional family orientated region. Valdemaras Rodzko CEO of Caerus said: “It’s such a delicate topic. Nobody’s shouting to the world about it. It’s very much kept in a close family or between partners. The end goal is to have a baby and people spend a lot of money to reach this goal.”
Linkevičius added: “That region faces more problems from the oxidative stress, and we are seeing higher levels over there.”
Lifestyle, hot climate and higher smoking habits in the Middle East are all causing higher rates according to Rodzko, and similar patterns are emerging in South Europe.
Pressure on females
Women historically faced immense pressure and blame when a couple struggled to conceive. They were subjected to invasive tests, questioned about their lifestyles, and unfairly held responsible for their partners’ infertility.
“If you don’t answer 50% of the problem, how do you get the extra percent success rate?” said Linkevičius.
“Pressure was focused on the female population and a lot of research was done for that gender. The male side of fertility was neglected, and now there is a multitude of research on female fertility, but still a lot of unknowns in male fertility. We hope the research our device is involved will build a better understanding of male infertility, and we think its awareness and interest is growing,” Rodzko commented.
Linkevičius added: “It’s a 50-50 problem. The bad thing about the male side of fertility is that most of the cases are unexplained. We know from the latest data that oxidative stress, it can explain a lot about these cases, up to 80% of unexplained male infertility cases relate to toxic stress.”
Infertility needs to be treated as an equal problem between potential parents so research and development of devices to address male infertility is a step in the right direction.
Diagnostic solutions like MiOXSYS can accurately assess sperm quality and quantity without invasive procedures, providing a less intimidating path to diagnosis.
Similar technologies are in development for Point of Care Testing (POCT). Brigham and Women’s Hospital Semen Analyzer is an automated, rapid, sensitive, and smartphone-based diagnostic tool that uses an optical attachment connected to a smartphone and a disposable device to assess a sample.
There are also a number of automated devices for male infertility such as the Japanese Organization for Medical Device Development Inc (JOMDD) AI-Assisted Automatic Sperm Sorting Device, Memphasys Ltd’s device Felix, Spermosens AB’s device JUNO and Lucendi Inc’s Semen Performance Analyzer. Also in development is Seragen Biotherapeutics Pvt Ltd’s SeraGel designed to collect semen samples and preserve the semen quality parameters.
Supplements and solutions
Discussing what to do to combat infertility, Rodzko recommended the following: “Eat less red meat, do less sport, less strenuous physical exercise, saunas, and keep away from cigarettes and other substances. You can do three months of a healthy lifestyle and compare your results to the previous test and see if you have a lower target. The diagnostic test allows you and your doctor to plan out that lifestyle depending on the results.”
Linkevičius added: “The key word is balanced here. You can also be too healthy, it’s very popular these days to do many things that seem to be healthy. Too much gym and other activities may have the opposite effect so it’s about working with your doctor to find that balance.”
Fertility is a two-way issue, and it requires both partners to take the right steps to conceive a healthy baby. It’s evident by the devices in development and on the market the stigma and awareness of male infertility is becoming openly subject and with this open discussion the opportunity to provide solutions are increasing especially as technology and our understanding of fertility evolves.