Brain-computer interface (BCI) developer Synchron said there were no serious adverse events in its 12-month Command study, which also showed reliable performance of the Stentrode implant. Synchron won FDA breakthrough device designation for the endovascular brain implant in 2020. The Command study is the first investigational device exemption (IDE) trial of a permanently implanted BCI, evaluating safety and efficacy in six patients with severe paralysis.
Synchron said the feasibility study’s results highlight its system’s “safety profile, stable signal performance, and reliable surgical delivery.”
Related: Toro Neurovascular’s catheter trial begins with first patient in Japan
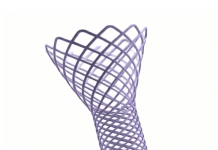
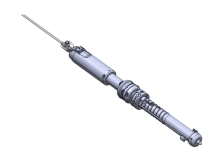
Instead of open-brain surgery like BCI rival Neuralink‘s implantation procedure, Synchron delivers its nitinol Stentrode implant with a catheter via the jugular and through the brain’s transverse sinus to the superior sagittal sinus for placement. The median deployment time in the study was 20 minutes.
Neurosurgeon Dr. Elad Levy presented the results today at the 2024 Congress of Neurological Surgeons (CNS) in Houston, Texas, calling them “a major medical milestone” in a statement shared with MassDevice ahead of his presentation.
“This minimally-invasive approach has the potential to unlock BCI technology at scale for the millions of patients with paralysis and other mobility challenges,” Levy said.
Levy is a co-principal investigator on the study as well as chair of neurosurgery at State University of New York at Buffalo and past president of the CNS Foundation. CNS is awarding Levy with the Duke Samson Award, which recognizes the best clinical paper addressing a topic of cerebrovascular surgery.
In addition to the study’s finding of no impact on the brain or vasculature in the six patients, the study also showed 100% accurate deployment for target motor cortex coverage, demonstrating consistent capture of brain signals related to motor intent and transformation of them into digital motor outputs (DMOs).
Those DMOs are “simple, thought-derived expressions of intent, converted into digital actions on computers” like scrolls, clicks and double-clicks, Synchron co-founder and CEO Dr. Tom Oxley said. “Making the DMOs easy to use, stable over time and generalizable across technology platforms, will unlock layers of independence and autonomy for patients.”
Synchron has recently shown amyotrophic lateral sclerosis (ALS) patients using the Stentrode implant to control Apple Vision Pro headsets, communicate with the help of OpenAI technology, and operate smart home devices with Amazon Alexa.
The Command study was supported by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative. The study was conducted at Mount Sinai Health System in New York City, University at Buffalo Neurosurgery and University of Pittsburgh Medical Center (UPMC) in collaboration with Carnegie Mellon University College of Engineering.
With the completion of the feasibility study’s initial follow-up, patients will start enrollment at additional sites next year.
Synchron now has five years of data from 10 research participants, Oxley said.