Currently there are hundreds of thousands of patients currently on waiting lists with little to no access to suitable donors.
Smart Reactors was co-founded by Brian Haddigan (CEO) and Mark Brassil (CTO) in 2019, both of whom have many years’ experience in medtech. They successfully built up the company to achieve profitability within 18 months of its formation. This is rare in medical devices, as it typically takes more than 10 years and many millions over multiple investment rounds. The company’s vision is to promote leading-edge biomaterials technological advancements, which includes biocompatible coating technology to support the long-term performance of blood contacting devices for applications such as cardiopulmonary bypass, ECMO, dialysis, cardiovascular, neurovascular, and peripheral vascular.
Related: icotec ag raises $30m in growth financing from MVM Partners
Blood contacting medical devices use a range of plastics, metals, and alloys. These materials have excellent mechanical and physical properties; however, they have variable hemocompatibility and when in contact with blood can lead to a pathophysiological reaction similar to traumatic shock. Therefore, minimisation of the activation mechanisms induced by the foreign surfaces used in blood contacting medical devices is of top priority.
This latest funding from EIC Pathfinder is a huge success story for Smart Reactors and will take the innovation in the company to the next level. The consortium, led by Smart Reactors includes the University of Galway (Ireland), University of Tubingen (Germany), Celllink (Sweden) and Brunel University (United Kingdom)
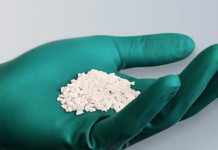
The technology will focus on the development of a green material extracted from wood pulp known as nanocellulose. This material is abundant, low-cost with encouraging human lung cells grow demonstrated in the lab. This approach will allow researchers to use nanocellulose as a scaffold for the development of engineered tissues that can perform the function of the of the lungs, while reducing the complications of the current state of the art equipment on the market today.
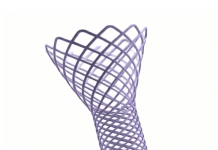
An artificial lung works by passing the blood of a patient over a membrane which adds oxygen and removes carbon dioxide from blood in a similar manner as the lung function. The materials used for this purpose today is made from plastic and is only capable of functioning for a short time before it needs replacement. Furthermore, it is extremely costly and requires extensive expertise. The challenge of designing an artificial lung device arises from the tendency of the blood to clot on the surface of this gas exchange mesh, however, Smart Reactors have the solution to this by using its hemocompatible technology, which was developed in locally in Galway and is commercially branded as Camouflage coating technology.
The purpose of the European research project is to support the design an artificial lung device that is based on the structure of the human lung, which is smaller, resistant to blood clotting and capable of functioning for extended periods without failing. The approach taken by Smart Reactors is to use lung derived cells to act as a barrier between the blood and a gas-exchange mesh made from nanocellulose, preventing clotting, and rendering the device more life-like.
Smart Reactors CEO Brian Haddigan said: “The development of an artificial lung is potentially of enormous benefit to patients with decreased lung function that are awaiting a lung transplant, helping these patients to breathe when their lungs are unable to do so. At Smart Reactors, we have built-up long-term relationships with key existing artificial lung manufacturers who are eagerly waiting for the development to evolve with huge interest.”
Dr Manus Biggs, lead engineer at the Centre for Research in Medical Devices (Curam) at the University of Galway, added: “Nanocellulose is a really interesting material from a bioengineering standpoint. It is cost effective, abundant and has very attractive properties that makes it suitable and attractive as a scaffold material for supporting lung cell growth in the lab. Importantly, it can be extracted from wood waste products, and is essentially a biodegradable, sustainable and green technology, which is of huge concern in the medtech industry right now as the healthcare sector contributes a staggering amount of waste and nearly 5% of all global carbon emissions.”
The project will be conducted over three years. Follow-on programs within the EIC funding model are in place to bring this project closer to commercialisation and patients after this initial phase.