Providence Medical Technology has received clearance from the US Food and Drug Administration (FDA) for its CORUS Posterior Cervical Stabilization System (PCSS), designed to treat up to three-level cervical Degenerative Disc Disease (DDD).
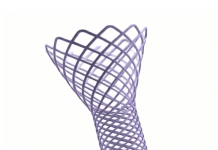
CORUS PCSS is posterior spinal instrumentation with integrated screw fixation aimed at providing immobilisation and stabilisation of spinal segments.
Related: FDA clears Orthofix Fitbone transport and lengthening system
Placed via a posterior surgical approach in up to three consecutive levels of the cervical spine (C3-C7), CORUS PCSS achieves bilateral facet fixation by spanning the facet interspace at every level with fixation points at each end of the construct.
It is intended as an adjunct to posterior cervical fusion (PCF) and to be used along with an anterior cervical discectomy and fusion (ACDF) at the same level.
Indicated for skeletally mature patients with DDD, CORUS PCSS is to be used with autogenous bone and/or allogenic bone graft.
This clearance is based on the results of the FUSE IDE study, which compared the safety and effectiveness of circumferential cervical fusion (CCF) as against the ACDF alone in patients with high-risk cervical fusion.
The FUSE IDE study, a multi-centre, randomised controlled trial, enrolled 227 patients across 18 US sites. Participants were aged between 18 and 80 years and suffered from symptomatic cervical DDD at three contiguous levels.
They were randomised to receive either the standard ACDF treatment or CCF (ACDF plus posterior cervical fusion) with the company’s PCSS technology.
Interim analysis of the study, with over 200 subjects at the one-year follow-up and 100 patients at the two-year follow-up, revealed a 44.3% higher composite fusion rate for CCF over ACDF, demonstrating the superiority of CCF in achieving fusion success. The dramatic difference in revision rates was also noted, with a significantly lower percentage of CCF patients requiring subsequent surgical intervention compared to those in the ACDF group.
At the two-year mark, the CCF arm exhibited a superior overall safety success rate, a secondary endpoint of the study. This was measured using a composite of fusion success, lack of subsequent surgical interventions, maintenance or improvement in neurological success, and improvement in the Neck Disability Index (NDI).
Additionally, the study found that a three-level CCF with PCSS had statistically lower procedure-related adverse events than a three-level ACDF.
The results from the FUSE study are significant, suggesting that the PCSS device could redefine the standard of care for patients with multilevel cervical DDD.
With minimal added operative morbidity, CCF with PCSS has been shown to improve long-term outcomes significantly when compared to the current standard of care.