Texas-based device company Autonomix Medical announced preliminary positive results from the proof-of-concept clinical trial evaluating transvascular radiofrequency (RF) ablation use in managing pain associated with pancreatic cancer.
Out of the first five subjects evaluated in the trial, 60% responded with a mean 6.33 reduction of pain on the visual analogue scale pain scale at seven days post-procedure. All members of the responder group had clinically meaningful pain relief at seven days post-procedure. Responder patients reported a mean 78% improvement in quality of health and a mean 45% improvement in quality of life after seven days.
Related: BaroPace pacemaker algorithm meets both primary endpoints in heart failure trial
The first five patients have been treated for procedural familiarity but will be excluded from the study’s objective analysis. Autonomix said the trial will enrol 20 subjects at a single clinical site, with the primary goal of the study to successfully target and ablate the nerves responsible for pain in pancreatic cancer patients using RF ablation via a transvascular method.
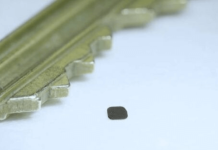
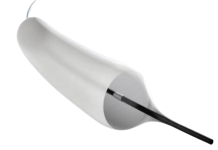
The company’s catheter-based technology is designed to detect neural signals linked to pain or disease and accurately target those nerves for treatment. There has been innovation in the pain management space in recent years, with the need for methods beyond opioids or invasive ethanol injections, which offer limited relief and carry significant risks.
Medical device giant Boston Scientific is a leader in the space, following the high-profile acquisition of Relievant Medsystems for $850m in September 2023. Relievant Medsystems had developed and commercialised a nerve ablation system for the treatment of a type of chronic back pain. Boston Scientific won US Food and Drug Administration approval for the Farapulse Pulsed-Field Ablation system in February 2024.
Autonomix’s chief medical officer Robert Schwartz commented on the preliminary data: “While these data will not be included in the final analysis, they provided our clinical team valuable insight into optimising the procedure, particularly the catheter entry point, where three of the five patients who saw a pain response had femoral access of the catheter and the two that did not respond had brachial access.
“We believe access factors played a role in the ability to ablate the appropriate nerves to see mindful pain reduction in the brachial access patients, as the bias of the catheter appears less optimal in ablating the target nerves from this approach to the target anatomy.”