Medical imaging company MolecuLight reported results from a recent independent clinical trial that evaluated the use of their fluorescence imaging device MolecuLight i:X to detect elevated bacterial loads in diabetic foot ulcers.
Over 500 million adults in the world have diabetes and it is predicted that there will be over 700 million adults living with diabetes by 2045. Almost 25 percent of people with diabetes will develop at least one diabetic foot ulcer during their lifetime. It is estimated that US Medicare spends around $28 billion to $98 billion annually on chronic wound care.
One of the challenges in wound care is the fact that clinically significant bacterial loads that develop in wounds are very difficult to detect and when they develop in wounds the healing process can slow or stop altogether. This is the clinical problem that MolecuLight is trying to address: to provide the only point-of-care medical imaging device to allow clinicians to safely visualize the presence and location of elevated bacterial loads so that they can best direct their wound care to remove those bacterial loads and help the wound heal.
How MolecuLight’s Fluorescence Imaging Device Works
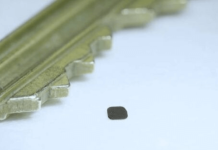
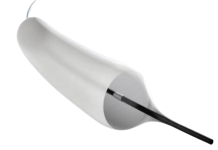
The hand-held device MolecuLight i:X emits violet blue light which is harmless to the human tissue. Using light stimulus from the device, Pseudomonas species that produce pyoverdines emit cyan fluorescence signals, bacteria that produce porphyrins emit red fluorescence, and elastin and collagen within the soft tissue emit green fluorescence. The components in the diabetic foot ulcer can be excited up to a depth of 1.5 mm.
In this way, the device acts as a diagnostic that identifies clinically significant bacteria above a pre-determined concentration by detecting natural fluorescence from bacteria cell walls. Therefore, a positive imaging result indicating that a diabetic foot ulcer is infected can be based on the presence of cyan or red autofluorescence signals from the wound bed or its periphery.
To properly use MolecuLight i:X, the room needs to be darkened as much as possible and the wounds need to be imaged at an ideal distance of eight to 12 cm from the wound. Disposable DarkDrapes are available to create dark environments for imaging wounds in rooms or settings where the rooms can’t be darkened.
Clinical Trial of MolecuLight i:X in Wound Healing of Diabetic Foot Ulcers
The single-center, open, parallel-group, prospective pilot randomized controlled trial involved 56 adult participants who had ulceration of the foot below the malleoli (a bone that is part of the ankle) and no suspected infection. Patients were randomly assigned to either standard treatment informed with bi-weekly autofluorescence imaging with the MolecuLight i:X device (29 patients), or standard treatment alone (27 patients).
The clinicians used the imaging findings to determine if additional treatment was needed. Most often the additional treatment involved further debridement (removal of dead, infected tissue or foreign debris from the wound) targeted to the regions of the ulcer with increased bacterial loads. Notably, there was no increase in antibiotics prescribed in the fluorescence imaging group.
The primary outcome was the proportion of ulcers that healed at 12 weeks. The secondary outcomes were reduction in wound area at four and 12 weeks, change in wound management decisions after fluorescence imaging and patient quality of life.
By the 12th week of the study, 45 percent of patients had a healed diabetic foot ulcer in the fluorescence imaging arm versus 22.2 percent in the control arm. The use of MolecuLight i:X doubled 12-week wound healing rates in diabetic foot ulcer patients compared to standard-of-care alone.
At the fourth week of the study, the median percentage wound-area reduction was 40.7 percent in the fluorescence imaging arm and 38.6 percent in the control arm. At 12 weeks, the median percentage was 91.3 percent in the fluorescence imaging arm versus 72.8 percent in the control arm.
Patients were 36 percent less likely to heal within 12 weeks if their wound was positive for increased bacterial levels at the start of the study.
No clinically meaningful differences were observed between groups with respect to patient quality of life.
The results of the MolecuLight i:X in wound healing clinical trial were published in the peer-reviewed journal Diabetes Care.
“We congratulate Dr. Russell [Associate Professor in Vascular Surgery at University of Leeds and lead author in the study] and the team at Leeds [West Yorkshire, England] for their excellent study and publication that shows the utility of MolecuLight to detect elevated bacterial burden and to inform clinical decision-making at the point-of-care,” says Anil Amlani, MolecuLight’s CEO in the company’s press release.
“A doubling of 12-week wound healing is a significant outcome and is consistent with what thousands of wound care clinicians are experiencing worldwide, that MolecuLight enables clinicians to deliver superior, proactive bacterial/infection management that improves wound outcomes,” added Amlani.
The Leeds Diabetes Limb Salvage service is currently using MolecuLight i:X to image all patients with wounds that are not achieving a healing trajectory within four weeks.
RELATED: US FDA grants expanded 510K clearance for MolecuLight’s i:X imaging device
The Next Steps for the Fluorescence Imaging Company
There are over 60 peer-reviewed publications showing the utility of the MolecuLight devices for a variety of wound care applications, as well as a number of clinical trials in progress using the MolecuLight i:X imaging device.
Currently, the medical imaging company is evaluating in a clinical trial in the UK if MolecuLight i:X can capture the presence of a bacterial fluorescent signature to predict a skin graft failure.
Another clinical trial at two US sites is recruiting participants to compare wound-area reduction of non-healing diabetic foot ulcers using MolecuLight i:X compared to standard-of-care treatment.